Treatment Option for Endometriosis: Excision Vs Ablation
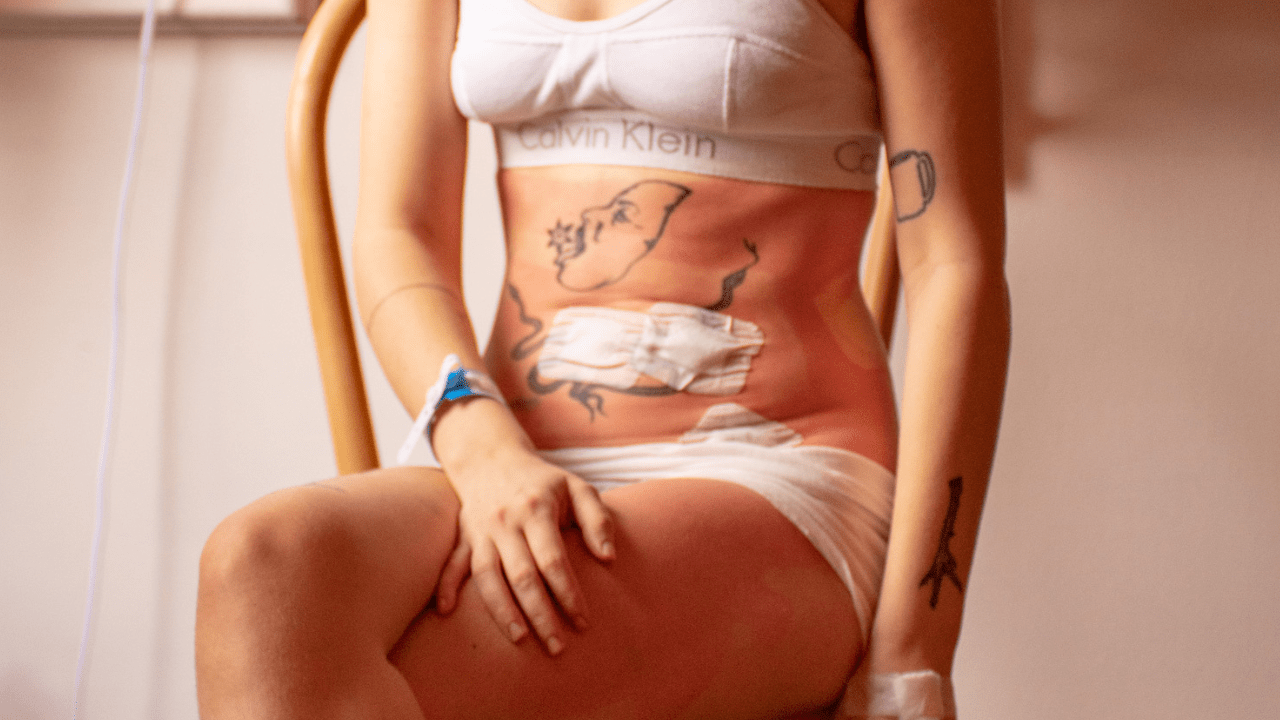
When I think about my journey with endometriosis over the last twenty years, I think of it as a beast that’s lived inside of me trying to take over mind, body and soul. Having tried the gamut of treatment options from dietary changes and physical therapy to hormones, medically induced menopause, and multiple surgeries, the beast continues to have a stronghold over me. As someone with lived experience who has undergone five surgeries in eight years, three of which were directly related to endometriosis, one of which was indirectly related, and all of which were considered ‘minimally invasive’, these surgeries are very complex, and intense experiences. But I’m alive and I’m here to make sure you’ve got all the information you need about endometriosis surgeries.
The only way to determine if someone has endometriosis with 100% accuracy and to gain a diagnosis, is by performing laparoscopic surgery. Laparoscopic surgery is an invasive procedure where doctors operate on a patient to look for endometriosis lesions. If lesions are found they are removed via either ablation (burning) or excision (cutting). Laparoscopy surgery is an option, especially if there is uncertainty about the diagnosis, lack of response, contraindication (ie. trying to conceive), an inability to tolerate medical therapies or invasive disease that is causing functional damage to organs (eg. bowel, ureter).
What is excision surgery for endometriosis
In trying to provide a comprehensive overview of the different types of surgery for endometriosis, it comes down to one of two options: excision and ablation. Excision involves the removal of endometrial tissue using cutting. When excision is used, the areas of the peritoneum (a sheet of smooth tissue that lines your abdominopelvic cavity and surrounds your abdominal organs) with endometriosis are excised (cut out). It allows the surgeon to cut underneath the endometriosis lesions to completely remove the endometriotic tissue, and does include cutting a small portion of surrounding healthy peritoneum.
Excision surgery is widely considered the gold standard when it comes to the treatment and removal of endometriosis.
What is ablation surgery for endometriosis
The other option for endometriosis surgery is ablation. Ablation involves destroying endometriosis tissue using heat, electricity, or another energy source, (so burning off the disease) while leaving the area of the peritoneum around the implants intact. Ablation may be effective for more superficial lesions, but it is not possible to remove deep infiltrating endometriosis (DIE) using ablation.
Including some diagrams here for visualization purposes highlighting the differences between the two options.
If you are a visual learner like me, the best way to picture the difference between excision and ablation is a weed. When a weed is growing out of the ground, you can rip it out of the ground where you see the stem meeting the grass; this would be similar to ablation. This technique of removing the weed leaves the grass intact, as well as the soil underneath the surface of the grass. With excision, you would instead use a spade or other tool to cut out the weed from the root. This affects not just the weed, but the surrounding ground, soil and grass as well ensuring a more complete and definite removal.

What happens during endometriosis surgery
Because of the invasive nature of the disease, it can affect multiple organs, as well as the peritoneum, and nerves. Surgeons will utilize a minimally invasive laparoscopic technique that could also involve robotic assisted technology. The goal of which, depending on the degree of severity, is to remove as much endometriosis, including lesions, adhesions and scar tissue, as possible. Biopsies will be taken throughout the surgery in order for pathological confirmation of endometrial disease.
Endometriosis surgery prep and aftercare
It’s important to note that surgery for endometriosis will look different for everyone. Whether this is your first surgery or your fourth, you want to try to give yourself as much time, grace, and healing as possible, both preoperatively and postoperatively.
Preoperatively, try to prepare your space as much as you can for where you will be when you are discharged from the hospital. Heating pads and ice are your friends. It is not recommended that you use heat directly on incisions immediately after surgery, but heat packs can help ease the pain in your shoulders/chest caused by excess gas trapped in your abdomen post surgery.
Try and have access to outlets for your electronic devices, and other items that need to be plugged in close by to your bed and/or couch. You want to try and limit as much unintentional abdominal movement as possible, as you will be quite sore in your midsection.
If you haven’t already, stock up on lots of comfy bottoms with forgiving elastic waist bands, like leggings, sweatpants, and pajama pants. You want to try and eliminate any unnecessary pressure to your abdomen in the ways of buttons and zippers. If you have a comfort item, like a stuffed animal or blanket, have them close by. Even as an adult, I find that inanimate objects can provide a lot of comfort in the setting of something as daunting and potentially traumatic as a surgery.
In my experience, noise-canceling headphones can be very helpful. Hospitals are quite loud and noisy places, with lots of beeps and whistles and bells. Having your favorite soundtrack to help calm your nerves and drown out some of the external commotion can be an often overlooked resource.
Regarding postoperative life, there are additional factors to take into consideration if you work for a living: how much time you can get off of work; what type of work you do (do you work from home, are you on your feet, do you have to get in and out of a vehicle frequently, do you have to lift or carry things); do you have other people in your life that you have to care for, including children and/or adults? Unfortunately, the way most insurance and hospital systems here in the US work, surgeries for endometriosis are classified as minimally invasive procedures and are more often than not same day procedures: meaning you are in and out of the hospital the same day. Obviously, there are exceptions to this, including surgical complications, other medical conditions and/or comorbidities that require inpatient post operative care, as well as how you are paying for the surgery (insurance, private, etc.).
Allowing your body to rest as much as physically possible post operatively is key to helping in your recovery journey. Not everyone has family members, partners, or support persons that can help with daily tasks like getting to/from the bathroom, bathing, and getting in and out of bed. And if you do, they may need some coaching on how to best support you. Mobility aids are your friend; they will look different for everyone, but canes and walking sticks, shower chairs, raised toilet seats, “squatty pottys”, and grabbers can be super effective in helping you navigate the first few weeks after surgery. Try and go for small, frequent walks throughout the day. Ambulating and getting your blood circulating is important to mitigate any risk of blood clots forming.
Most importantly, listen to your body. Don’t overdo it and if something doesn’t feel right, contact your care team. Remember, healing is not linear, and it will look different for everyone.
Potential risks of endometriosis surgery
Regardless of comorbidities (meaning other health conditions that can make having surgery more complicated), surgery takes a very real toll. Anesthesia alone is a very powerful procedure, and the amount of time it takes for your body to recover from being under is significant. And while surgery for endometriosis might help one symptom, it could unintentionally but unfortunately cause another. Post operative pain in and of itself is a very real factor to consider. Additional risks include infection, bleeding, nerve damage, and damage to organs.
While the goal of surgery is to excise and/or ablate endometrial lesions, so as to remove disease from the body, endometriosis is a progressive and recurrent disease. In other words, disease can 1) persist after surgery, as it is impossible to get all of it out due to where it is located and how obscured it is and 2) it can come back. The reality of surgical interventions is that it can end up being a cyclical process, as surgery creates scar tissue, of which endometriosis will attach to, causing the need for additional surgeries. From my perspective, the most important takeaway for someone with an endometriosis diagnosis facing the various, albeit limited, treatment options, is realizing that unfortunately, there is no cure for endometriosis, including surgery.
As with any medical related decision, shared decision making with your healthcare team should be paramount in how and when you decide to have surgery. Seeking second, third and fourth opinions is in your right as a patient. There are a number of factors to consider when making a decision to have surgery, including what kind of surgery to have, who to have surgery with, where to have your surgery, how to pay for it, and what life will look like for you postoperatively. You are the driver when it comes to which direction to go next, so no matter how overwhelming it may seem, know that you have the ability to make choices in your care and treatment.
If you or someone you know thinks they may have endomestriosis and has not yet been diagnosed you can take a free endometriosis risk assessment test HERE.
Madalene Zale (she/her) is a public health and health equity professional and researcher. She has worked in healthcare for over 12 years and has her master’s in public health. As a patient with lived experience, living with multiple chronic illnesses including endometriosis, she aims to shed light on the many facets of life as a sick person. Endometriosis affects so many people in so many ways: as both a patient and researcher, she understands the importance of cultivating awareness around endometriosis, in the hopes of improving health outcomes for everyone suffering from this debilitating disease.
References
Excisional versus ablative surgery for peritoneal endometriosis - PMC (nih.gov)
Role of surgical treatment in endometriosis - PubMed (nih.gov)
Recurrent Endometriosis | SpringerLink
Surgical Scar Endometriosis: An Emerging Enigma - PMC (nih.gov)
Effects of Anesthesia - Brain and Body | Made for This Moment (asahq.org)
Complications following surgeries for endometriosis: A systematic review protocol - PMC (nih.gov)
Laparoscopic surgery for endometriosis - PMC (nih.gov)
Clinical diagnosis of endometriosis: a call to action - ScienceDirect
Peritoneum: Anatomy, Function, Location & Definition (clevelandclinic.org)
4 Women with Endometriosis are Leaning on Canes for Mobility Support (sheknows.com)
Previous Article All Articles Next Article
All Articles


