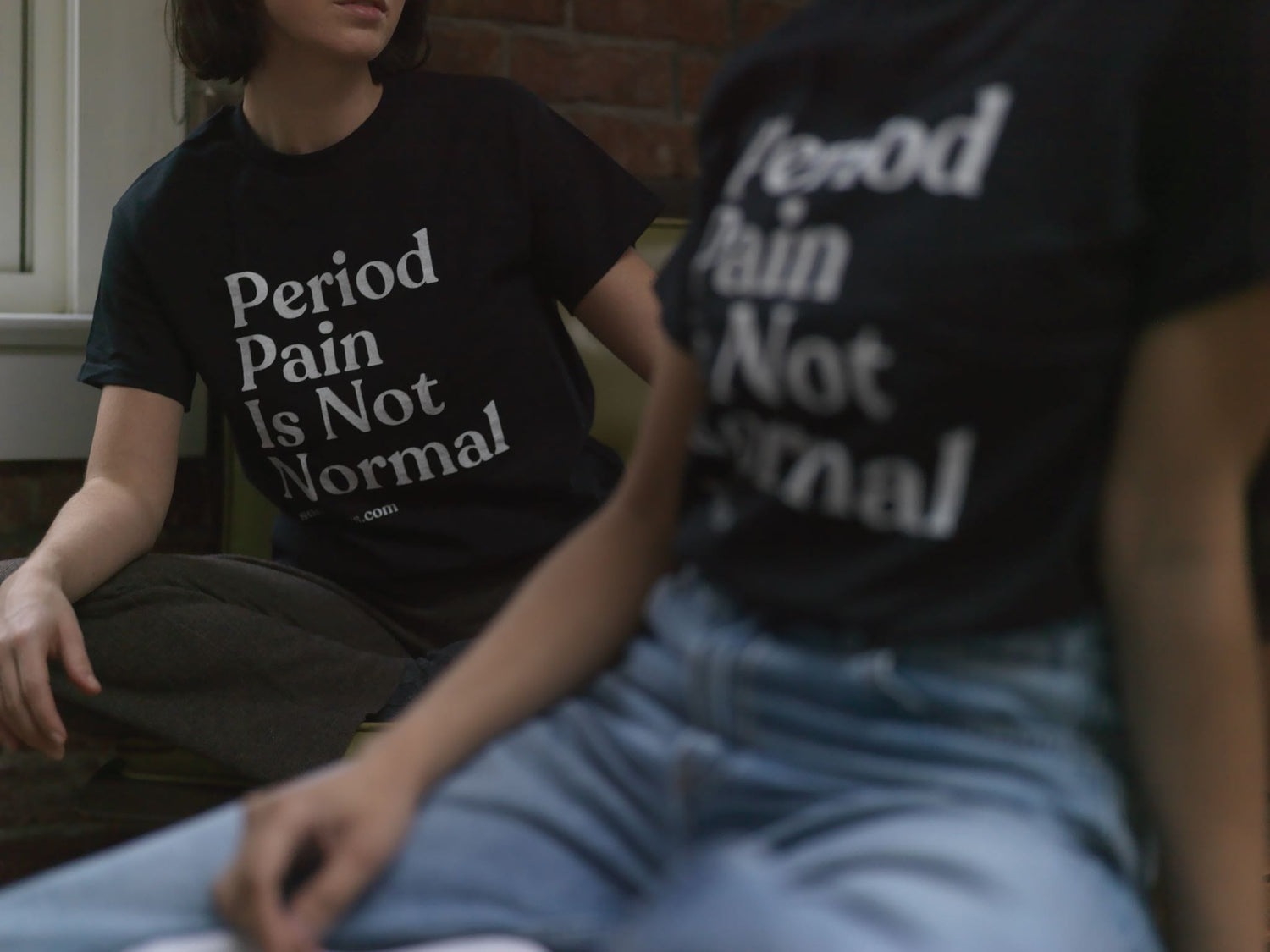
Debunking Myths About Period Pain: What’s Normal and When to See a Doctor
I remember the first time I experienced excruciating period pain. I was in my early twenties, sitting at my desk at work, trying to power through what I thought was just a "bad period." I kept telling myself it was normal—periods are supposed to hurt, right? Little did I know, my severe pain was far from typical and a sign that something more was going on.
Period pain is something many of us have learned to live with, especially those who are dealing with endometriosis, adenomyosis or another menstrual disorder. Still, there’s a lot of misinformation out there about what’s normal and what might be a red flag. In this post, we’ll debunk common myths about period pain, discuss what constitutes normal period pain, and guide you on when to see a doctor.
Myth 1: All Period Pain Is Normal
Debunking the Myth: It’s easy to brush off period pain since we’re told it’s just a part of menstruating, but not all period pain is normal. Mild discomfort, cramps, and achiness are common and generally nothing to worry about. However, severe, debilitating pain that interferes with your daily activities is a different story.
What’s Normal: Normal period pain, or primary dysmenorrhea, usually starts a day or two before your period and may last for two to three days. It often feels like mild to moderate cramping in your lower abdomen, and while uncomfortable, it shouldn’t stop you from going about your day.
When to See a Doctor: If your period pain is severe enough to disrupt your daily routine, or if you’re relying on painkillers to function every month, it’s time to consult a healthcare professional. Conditions like endometriosis, fibroids, or adenomyosis could be the underlying cause of your pain, and early diagnosis is key to managing these conditions effectively.
Myth 2: You Just Have to Live with Period Pain
Debunking the Myth: Many of us have been conditioned to believe that period pain is just something we have to endure. While it’s true that some discomfort is common, you don’t have to suffer in silence.
Natural Pain Relief Options:
- Cramp Cream: This fast-absorbing cream provides targeted relief from menstrual cramps. Its blend of ten natural ingredients, including arnica and wintergreen, helps soothe muscle pain and inflammation.
- Heat Pad: Applying heat to your lower abdomen can relax the muscles that cause cramping. The Somedays Heat Pad is designed to provide consistent warmth through its cozy, pelvis-shaped design.
- Solace Soak: A warm bath with Solace Soak can help ease tension and reduce pain. The magnesium, arnica and essential oils work together to relax your body and mind, making it easier to cope with period discomfort.
- Castor Oil Set: A traditional castor pack with a modern twist to support hormone health and reduce period pain. This science-backed treatment is a game-changer for painful cycles and mood swings.
Myth 3: Period Pain Gets Better with Age
Debunking the Myth: While some people may notice that their period pain improves after having children or as they get older, this isn’t the case for everyone. In fact, for some, period pain can worsen over time, especially if they develop conditions like fibroids or endometriosis.
What’s Normal: There’s no universal rule that period pain will improve with age. Your menstrual cycle can change over time, and it’s important to pay attention to any shifts in pain or symptoms.
When to See a Doctor: If your period pain worsens as you age or you start experiencing pain during other times in your cycle (like ovulation), it’s worth discussing with your doctor. These changes could indicate a new underlying condition that needs to be addressed.
Myth 4: Heavy Bleeding Is Normal with Period Pain
Debunking the Myth: Heavy bleeding and severe pain often go hand in hand, but neither is something you should ignore. Heavy menstrual bleeding (menorrhagia) could be a sign of an underlying issue like fibroids, polyps, or a bleeding disorder.
What’s Normal: A normal menstrual flow is about 30-40 milliliters of blood per cycle. If you’re soaking through a pad or tampon every hour or passing large clots, this is considered heavy bleeding and is not typical.
When to See a Doctor: If you’re experiencing heavy bleeding along with severe pain, it’s crucial to see a healthcare provider. They can run tests to determine the cause and provide you with the appropriate treatment options.
Understanding what’s normal when it comes to period pain is crucial for your health. While some discomfort is common, don’t ignore severe pain or heavy bleeding—these could be signs of something more serious. If you’re unsure whether your symptoms are normal, it’s always best to consult with a doctor. And remember, you don’t have to tough it out—natural pain relief products can make a significant difference in managing your period pain.
Taking charge of your menstrual health means knowing when something is off and seeking help when needed. Don't hesitate to reach out to your healthcare provider if you suspect your period pain might be more than just a "bad period."
Think you may have endometriosis but haven’t been diagnosed? Take our free endometriosis assessment available HERE.
Join our Betterdays community - a weekly newsletter where we break down the latest (TLDR) news, research and breakthroughs related to your reproductive health—with a splash of humor to get you through the tough days.
Previous Article All Articles Next Article
All Articles


